Foot Surgeries
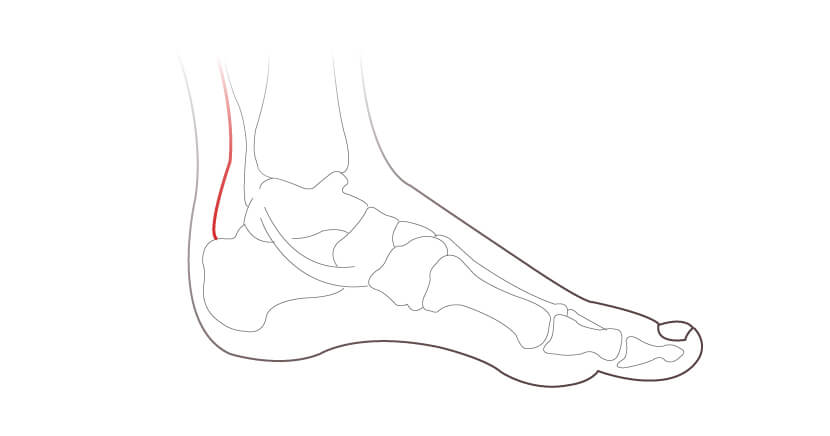
An Achilles Tendon Repair might be suggested if your specialist suspects a rupture. Prior to surgery an Ultrasound or MRI will be carried out to assess the extent of damage and the gap between the tendon ends.
The surgery helps to restore normal anatomy and function of the achilles. An incision will be made at the back of the calf and the two torn ends attached together with a strong suture. If there is severe damage then a part of the tendon may be removed and replaced with a healthy tendon from another part of your foot.
Where possible, the procedure will be carried out through a minimally invasive technique where 2-3mm incisions will be made. This will help reduce possible complications during recovery.
If you have a job that does not require significant physical activity, then you can continue working after 1-2 weeks. If you have an active job then you may need to wait 6-8 weeks before returning to work. Your specialist will run through your recovery plan during your consultation. It may take 6-12 months to gain sufficient strength to return to sports or significant physical activities requiring exertion.
Surgery for Ankle Arthritis
If ankle arthritis does not respond to conservative measures then surgery may become the recommended course of treatment.
Ankle Arthritis Surgery
Your surgeon will recommend the most appropriate type of surgery based on your particular case. These might include:
An ankle arthroscopy may be advised to treat ankle arthritis that is caused by debris from torn cartilage or from a bone chip. There may bone spurs at the front of the ankle that cause pain or restriction in movement.
The arthroscopy procedure uses a fiber-optic viewing camera to allow for minimally invasive surgery, this in turn reduces recovery. With the use of the camera, 2-3mm small incisions will be made followed by repair of any cartilage damage, removal of bone spurs and fixation of ligaments.
The minimally invasive procedure allows early mobilisation in most cases. Weight-bearing is allowed immediately in a protective shoe or boot. Return to full activity can be anything from 4 to 8 weeks depending on the level of surgery and damage repaired. It may be a few months before you may return to sporting activities. Crutches might be used initially to help mobilise in the first couple of weeks.
In more severe cases an ankle fusion may be suggested to assist with ankle arthritis. This is where two or more of the bones in your ankle are fused into one piece with the use of a screw fixation. Where possible, minimal invasive surgery will be carried out, small 2-3mm incisions would be made and the procedure carried out with the assistance of a camera.
Post-operative recovery after an ankle fusion procedure requires a below knee cast and no wait to be put onto the ankle for approximately eight weeks. Careful mobilisation is required over the next couple of months and it might be 6 to 12 months before any significant physical activity, such as sports, is allowed.
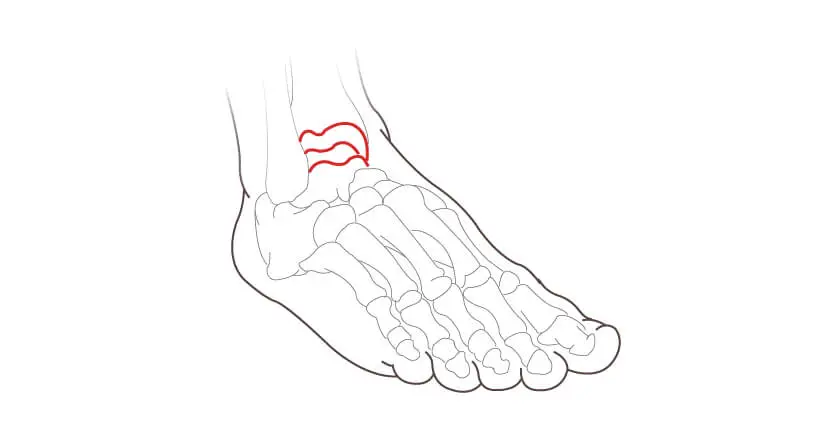
The Brostrom-Gould Ankle Stabilisation is a widely used procedure for treatment of lateral ankle sprains, where the ligament on the outside of your ankle is repaired. This would typically be carried out following a twist or sprain to your ankle where the ligament has become torn or stretched.
The stretched or injured ligaments are repaired using an Arthrex Ankle Brace, this allows faster recovery. Key-hole ankle surgery may also be performed to treat subsequent damage to a chronic injury.
Following surgery you should be able to mobilise almost immediately with the use of an air cast boot, which you’ll need to wear for the first three weeks. The total recovery takes six – eight weeks.
Modern fixation techniques with an internal brace and anchors have allowed surgeons to improve the post operative rehabilitation following ankle ligament repair, allowing predictable recovery and a quicker return to sports.
Ankle impingement can develop in the front or back of the ankle region following a sprain. This is where a bony growth forms which restricts range of motion in the ankle.
Anterior Ankle Impingement
Anterior Ankle Impingement, also known as footballer’s ankle, is where the impingement is located at the front of the ankle.
Symptoms may include:
- Pain when pulling toes towards your body
- Clicking sensation in the front of your ankle
- Weakness in the ankle
During the procedure your surgeon will make two small incisions at the site of the impingement, using an arthroscope. They will then identify the thickened tendon or ligament. A small shaver is used to remove any thickened or inflamed tissue, alongside any bone spurs that may be present.
Following the surgery you’ll be provided with an ankle splint and crutches to be used over the first one-two weeks. You’ll be able to gradually increase activity during this period. It will take four-six weeks before you can return to normal activities.
Posterior Ankle impingement
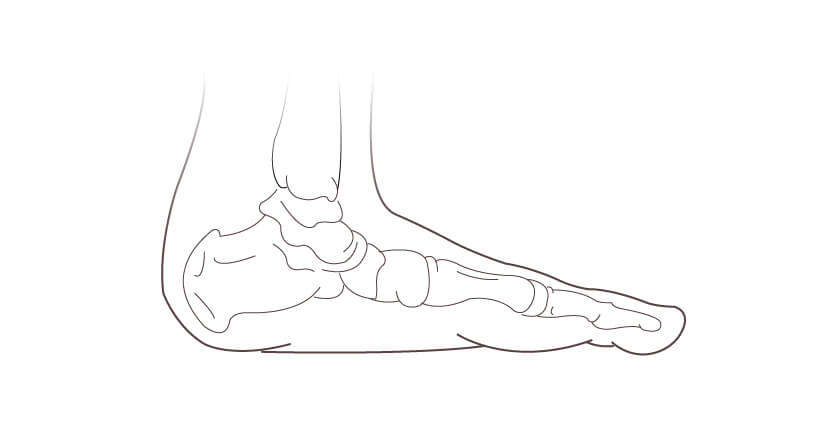
The ankle bone (talus) sits on the heel bone (calcaneus), forming a secondary joint in the ankle (the subtalar joint). At the back of the ankle bone there are two small bony lumps (tuberosities), one on the inside and one on the outside. In about 15% of people, the outside lump is naturally separated from the talus, and is called the Os Trigonum.
The Os Trigonum can cause problems in people who regularly point their feet downwards sharply, it is most common in ballet dancers. When the Os Trigonum gets pressed between the bottom edge of the shinbone (tibia) and the top surface of the heel bone, the tissues above and below the Os Trigonum can become trapped, leading to inflammation and swelling.
The Os Trigonum can be removed through a small incision at the back of the ankle. Typically you will require rest at home for non manual jobs, where you will use a back slab and crutches.
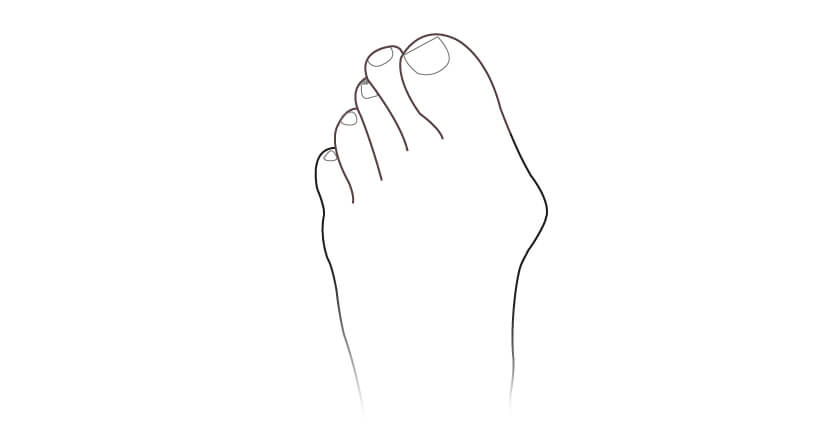
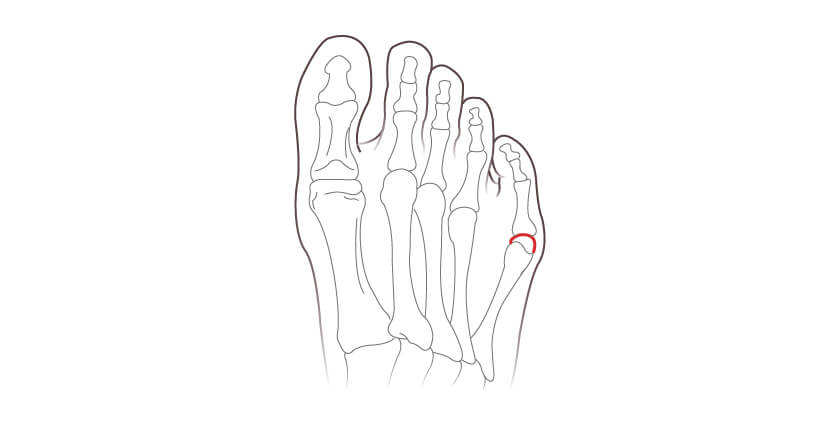
What is Bunion Surgery?
Bunion surgery is a type of surgery that is performed to correct a bunion. Bunion (Hallux Valgus) is a foot deformity / bony bump that results in prominence of the inner part of the big toe joint, in particular at the base of the joint where the big toe meets the first metatarsal bone. Bunions can cause pain, swelling, and difficulty walking, and may become worse over time if left untreated.
During bunion surgery, the Bunion surgeon may remove some of the bone or tissue from the affected joint to realign the toe and relieve pressure on the bunion. The procedure may involve making an incision in the skin over the bunion, and then cutting and repositioning the bones to correct the alignment.
There are several different types of bunion surgery, and the specific procedure used will depend on the severity of the bunion and the individual patient’s needs. Recovery time for Bunion Surgery can vary depending on the type of surgery performed and the extent of the correction needed. It is important to discuss the risks and benefits of bunion surgery with your doctor to determine whether it is the right option for you.
Our bunion surgeon, Mr Kaser Nazir, specialises in the minimally invasive bunion surgery. We will outline further details on the types of bunion surgery and what it involves, including postoperative recovery from Bunion Surgery week by week and typical pricing for bunion correction in London, UK.
What are the Advantages of Bunion Surgery?
A bunion, or hallux valgus deformity, affects the big toe. The aim of bunion surgery is to:
- Completely correct the underlying misalignment of the bones and ligaments causing the deformity.
- Appropriately realign the joint to ensure minimal risks of recurrence of the bunion.
- Improve function
- Relief from pain
- Cosmetically pleasing appearance
Types of Bunion Surgery
There are several different types of bunion surgery, and the specific procedure used will depend on the severity of the bunion and the individual patient’s needs. Some common types of bunion surgery Our central London based bunion surgeon, Mr Kaser Nazir, primarily assists with:
- Minimally invasive bunion Surgery, also known as “Keyhole Bunion Surgery”.
- Scarf and Akin Osteotomy
- Lapidus Procedure for more severe bunions
Day case minimally invasive keyhole Bunion surgery allows immediate weight-bearing with very little postop of pain and quicker recovery than traditional Bunion surgeries. Mr. Kaser Nazir has an international expertise in keyhole Bunion surgery and is one of very few surgeons in the United Kingdom with significant expertise in this operation.
Bunions can cause the whole foot to deform with dislocated toes and painful deformities! Day case operation performed by Kaser Nazir for this patient who travelled from Mauritius to have the operation under a local anaesthetic block in London. #bunion #halluxvalgus #footsurgeon #bunionkinguk #bunionkingoflondon #bunionsurgeon #bunion surgery
Keyhole bunion surgery by Kaser Nazir performed for a painful deformity that progressed quickly. This is the only permanent fix!! #bunion #halluxvalgus #footsurgeon #bunionkinguk #bunionkingoflondon #bunionsurgeon #bunion surgery #bunionspecialist #footsurgery #designershoes #footclinic #kasernazir #toesurgery #footsurgeon #footclinic #beautifulfeet #keyholebunion #harleystreet #cosmeticfootsurgery #chanelshoes #londonfoot
Bunions: Diagnosis, Cause and Treatment
Bunions often develop over a long period. They are progressive, meaning that without intervention a Bunion will get worse over time. A Bunion will typically first appear as a mild bump below the big toe that protrudes out from the foot. As it develops the bony bump may become more severe, causing irritation in footwear, redness and inflammation. As the joint deviates further, the big toe may start to underride or overlap the adjacent toes, causing further issues and painful symptoms.
Know more about Bunions: Diagnosis, Cause and Treatment
A bunion or hallux valgus deformity is more common in women than men and is often a hereditary issue. Bunions can also be caused by narrow fitting footwear or high heels, where the toes can be pushed together and put pressure on the big toe.
It is worth visiting a podiatrist or a foot surgeon specialising in bunion surgery when you see a bunion starting to develop, they can assist with advice and conservative treatment including:
- Custom orthotics
- Toe splints
- Advice on appropriate footwear
Whilst splints and orthotics can slow down progression of the bunion, the deformity can not be corrected without surgery. If you find that your bunion symptoms are deteriorating or become pain and you can’t wear the shoes you would like to then it is time to arrange an appointment with a bunion specialist.
On arranging a consultation with Mr Kaser Nazir to discuss bunion surgery, we will also schedule an X-ray appointment.
Bunion Symptoms:
Clinically signs of a bunion include:
- Swelling, redness or pain around the big toe joint
- A bump at the side of the base of your big toe
- Pain under the ball of the big toe or often the second toe due to the bunion pushing it over
- Widening forefoot
- Difficulty wearing closed shoes comfortably
X-ray examination of the bunion may confirm:
- Bone displacement
- Joint swelling
- Bone overgrowth
- Big toe joint arthritis
- An increases angle of the hallux valgus (big toe)
- An increased angle between the first and second metatarsal, thus a wide foot
- Flat foot associated with bunion
- Quality of bone and osteoporosis
Bunion surgery has come a long way from the old traditional bunionectomy. The recovery following a minimally invasive bunion surgery is much quicker and will not require a cast.
Though there are many types of bunion surgery, Mr Kaser Nazir typically suggests either:
- Minimally invasive bunion correction or keyhole bunion surgery for most bunions with good quality bone and minimal or no arthritis evident on X-rays.
- Scarf and akin osteotomy for mild to moderate bunions, very slim bones or with osteopenia.
- Lapidus procedure for severe bunions deformities with arthritis of the midfoot or severe hypermobility (least common).
- Big toe joint fusion for those with arthritis and bunion deformity of the big toe (rare).
Mr Kaser Nazir also specialises in arthritic bunion issues. Visit our big toe arthritis page for further information.
Bunion Surgery Costs
Mr Kaser Nazir is covered by all major insurance companies. If you plan on using medical insurance please contact your provider and request authorisation for a consultation and X-ray. Following your appointment, our team will provide you with details on how to authorise the surgery.
If you are privately funding your appointments and procedure, the cost of bunion surgery will depend on which type of bunion surgery is recommended. This will vary depending on the severity of your bunion. Below is a guide to the bunion pricing:
Consultation with Mr Kaser Nazir: £250
Preoperative X-ray one foot: £160
Bunion correction for one foot under sedation:
Minimally invasive bunion correction: From £5,732
Scarf and akin osteotomy: From £5,395
Lapidus procedure: £8,255
Postoperative X-ray one foot: £160
Please note that the above fees are approximate, fees may change depending on Mr Kaser Nazir’s recommendations.
The Lapidus procedure will require additional postoperative fees including cast changes and an aircast boot.
How each Bunion Procedure is Performed
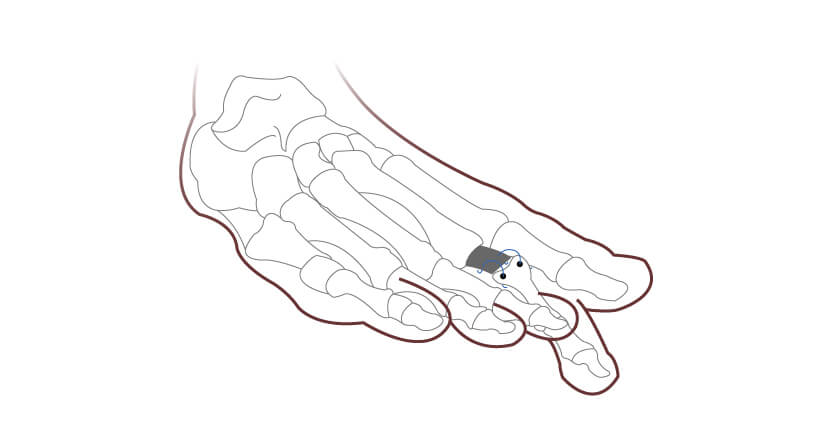
Minimally Invasive Bunion Surgery
Minimally Invasive Bunion Surgery, also known as Keyhole Bunion Surgery, uses specialised burrs that are used to cut and reset the metatarsal and proximal phalanx bone into a corrected alignment alongside specially designed screws through very small incisions.
Mr Nazir typically uses the PECA bunion correction system. The procedure is carried out with the aid of an X-ray machine and specialised instrument to accurately calibrate the required bunion correction. This allows the bunion surgeon to make three – four 2mm incisions and minimises the damage to the soft tissue.
Advantages of the minimally invasive bunion surgery include:
- Less downtime
- Less swelling
- Minimal postoperative pain
- Less chance of joint stiffness due to reduced trauma
Why is a screw fixation still required for the minimally invasive bunion correction?
Research shows that without a fixation keeping the joint in place once the bones have been realigned increases the risk of complication such as delayed or non-union of bones and recurrence of the deformity. Using the PECA correction system with screws significantly reduces the chance of the bunion recurring and predictable recovery, including immediate weightbearing with minimal pain and swelling.
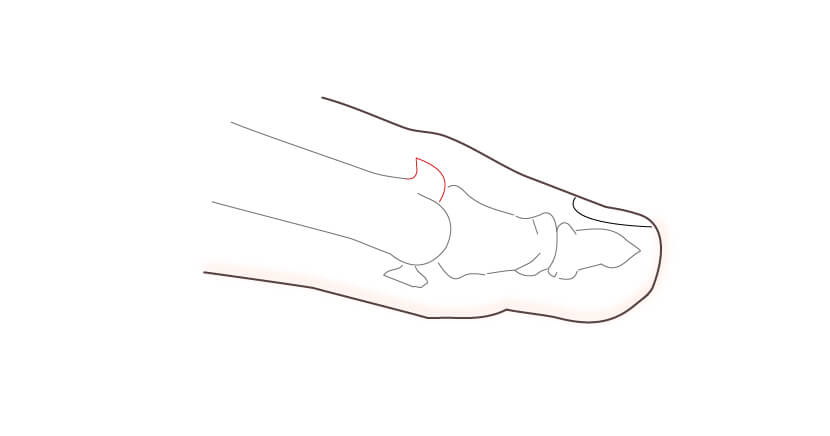
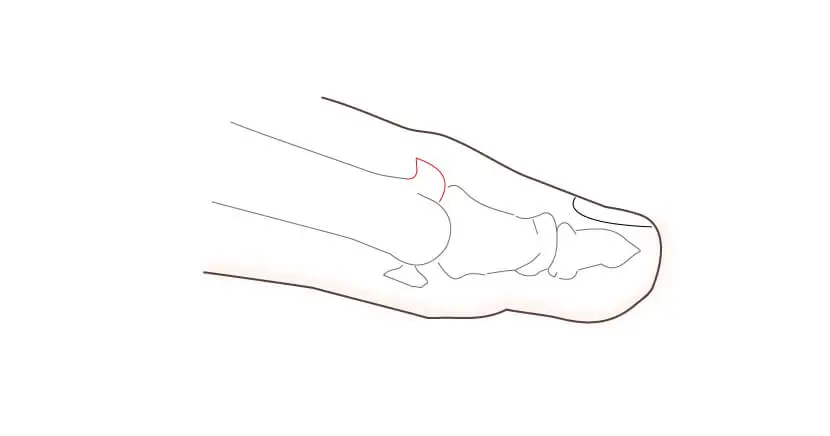
Steps of the minimally invasive bunion surgery
Step 1: A small 2mm incision is made on the inner side of the foot allowing the first metatarsal to be cut using a cutting burr known as a Shannon.

Step 2: The head of the first metatarsal is repositioned, to minimise the bony prominence. The Pecaplasty jig device is used to secure the corrected bones temporarily and checked on X-rays.

Step 3: Two screws are used to fix both sections of the metatarsal in its new position.

Step 4: A wedge is sometimes removed from the first proximal phalanx to reposition the big toe into a straighter natural alignment if required. This is also fixed in place with a screw.

Step 5: The protruding bone is cut away and flattened to a natural outer arc.

Recovery following the minimally invasive bunion surgery

Scarf and Akin Osteotomy
The scarf and akin osteotomy is a one of the most popular types of bunion surgeries as it:
- Restores foot mechanics
- Allows for correction of small and moderate deformities
- Low recurrence rate
The procedure is carried out using titanium screw fixations that hold the big toe in the corrected position whilst the foot heals. It has a good long-term evidence base with predictable and repeatable excellent outcomes.
Steps of the scarf and akin osteotomy
Step 1: An approximately 8cm incision is made on the inner side of the bunion joint. The soft tissues are released to expose the bunion joint.

Step 2: The Bunion prominence is shaved using a bone saw.

Step 3: Metatarsal bone is cut and joint is realigned, then screwed in place using 2 titanium screws.

Step 4: A small wedge is removed from the phalanx to straighten the end of the toe (Akin Osteotomy)

Step 5: The phalanx is fixed together with a further titanium screw where the wedge has been removed, promoting a correct alignment of the toe

Recovery following the scarf and akin osteotomy

The Lapidus Procedure for Bunion Surgery
The Lapidus procedure is carried out to correct more severe bunions or for patients who have a bunion and suffer from hypermobility. Patients who are hypermobile have an increased chance of recurrence following other bunion techniques.
Steps of the Lapidus procedure
Step 1: An incision is made at the side of the foot measuring 13-15cm.
Step 2: The soft tissues around the bunion and midfoot joint are released to expose both the big toe bunion joint and the midfoot joint.
Step 3: The bony growth of the inner bunion is removed using a bone saw.
Step 4 The joint near the instep (tarsometatarsal joint) is removed, realigned and fused with a fixation which includes screws and a plate.
Recovery following the Lapidus procedure

Find out further pricing information through our quote generator
Contact our team on 02078208007 or email admin@londonfootandanklesurgery.co.uk if you have any questions regarding pricing.
Finance Option Available
Our bunion procedures are carried out at The Weymouth Street Hospital who have partnered with Chrysallis Finance to offer monthly payment plans for surgery.
Following your consultation we will provide a full breakdown of your procedure fees so you can arrange your preferred finance option.
Bunion Surgery: Frequently Asked Question
Keyhole bunion surgery, or minimally invasive bunion surgery, is a modern technique to surgically correct a bunion. The procedure is carried out with the aid of a live X-ray machine to cut and reset the bone malalignment using 3-4 small 1 to 3mm incisions to guide the specialised surgical instruments and fix the bones in the corrected position using specialised screws designed for bunion correction.
As there is minimal scar tissue, the area heals much quicker than more traditional bunion correction. Mr Kaser Nazir has seen excellent results with his patients who have reduced pain and quicker recovery.
Mr Kaser Nazir is the leading bunion surgeon based at 17 Harley Street in central London. He specialises in the minimally invasive/ keyhole bunion correction and is internationally recognised for performing this operation.
Discomfort from a mild bunion can be helped with a toe splint, custom orthotics or wider footwear. Some mild bunions can also require surgical intervention if they are painful.
There are a few procedures that may be suggested, such as the scarf and akin osteotomy or lapidus procedure for more severe bunions. Mr Kaser Nazir, however, can carry out the minimally invasive/ keyhole bunion procedure that provides an excellent cosmetically pleasing result, with reduced pain and recovery.
Early signs of a bunion may include:
- Swelling, redness or soreness around the big toe joint
- Limited movement of the big toe
- A bump on the outside of the base of your big toe
- Stiffness in the big toe joint
- Pain under ball of second toe due to overloading
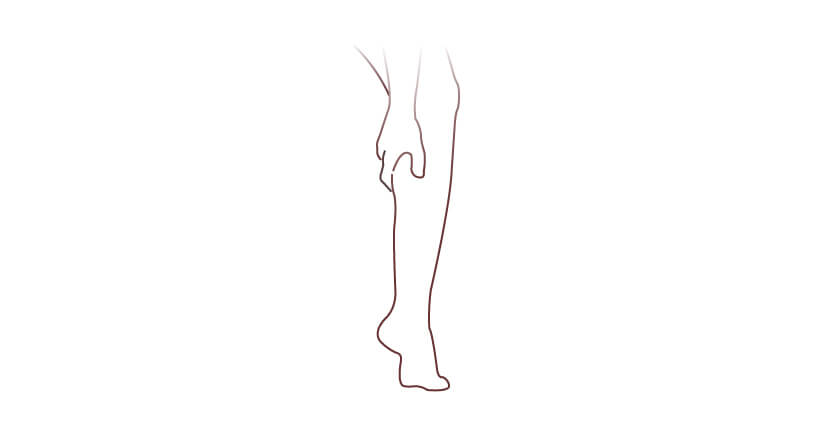
Calf Surgery
Surgery is rarely needed to treat calf pain. Calf surgery may be recommended only after conservative treatments fail to relieve symptoms and most often to resolve tightness that is leading to secondary issues, such as foot and ankle pain.
Surgery to Lengthen Calf Muscle
Surgically resolving calf tightness is known as a gastrocnemius recession:
Gastrocnemius Recession
A Gastrocnemius recession is typically carried out due to equinus contractures, where you are unable to put your foot in neutral position due to tightness of the calf muscles and/or tendons in the calf. The aim of the procedure is to lengthen the calf muscle to create greater flexibility. The procedure is commonly accompanied by the HyProCure or general flat foot correction and chronic achilles or forefoot problems that are associated with overly tight calf muscles.
Initially your podiatric surgeon will make a small incision to the inner calf, half way between the knee and the ankle. The muscle is then lengthened. No fixations (wires, screws, implants or pins) are used during this procedure.
You will need to take six-eight weeks off from non manual work and eight-twelve weeks off from manual work. You will use a cast for the first two-four weeks following surgery whilst non weight bearing. Following this you will be provided with an Air cast boot to mobilise in for a further two weeks. At three-six months you should be able to continue with high impact activities, such as the gym and running.
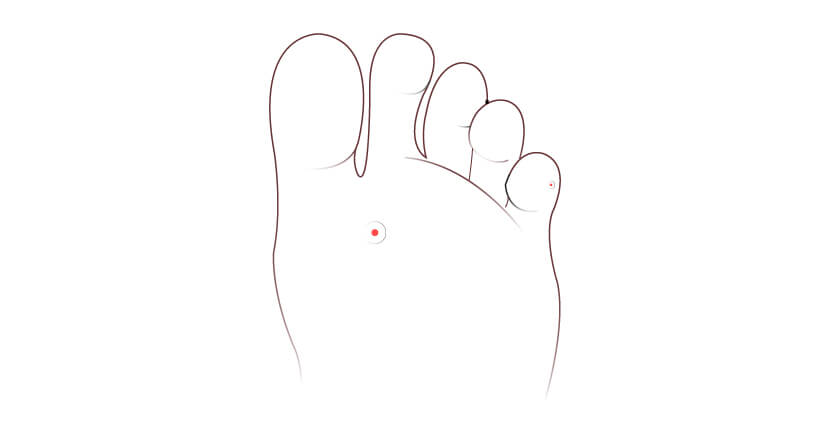
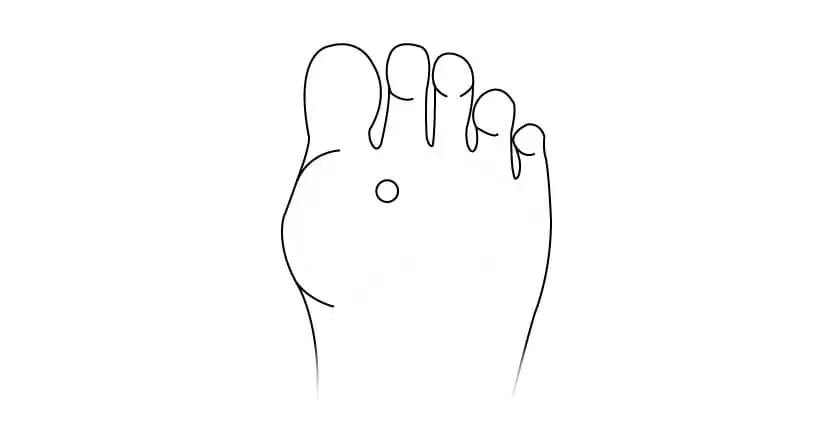
Corn and Callus Excision
Surgical removal of corns is advised when there is burning pain or the patient is concerned that they have developed unsightly lumps over the small joints of their toes.
An elliptical incision is made over the corn allowing the full depth of the corn to be excised as well as the fibrous scar tissue and bursal tissue that is often present.
In some cases surgical corn removal is not suggested due to the size of the corn or the fact that it is caused by deformity of the toe. In such cases, correction of the toe to shorten or straighten the toe may also be recommended instead to avoid the risk of recurrence. Click here to find out more on toe correction.
What is Corn Removal Surgery?
Corn removal surgery is a medical procedure that involves the surgical removal of corns, which are areas of thickened skin that develop on the feet due to constant pressure or friction.
Corns typically occurs on the toes, ball of the foot, or heel, and can be painful and uncomfortable. Corn removal surgery is performed by a qualified healthcare professional, such as a podiatrist or a foot surgeon, and aims to alleviate pain, improve foot function, and prevent recurrence of corns.
Who is a Candidate for Corn Removal Surgery?
Candidates for corn removal surgery are individuals who have persistent corns on feet that do not respond to conservative treatments such as wearing proper footwear, using padding or orthotics, and applying over-the-counter corn removers.
Candidates may also have corns that are causing severe pain, discomfort, or affecting their daily activities. Additionally, individuals with deep-rooted corns or corns that are associated with structural abnormalities of the foot may also be candidates for corn removal surgery.
A healthcare professional can determine the candidacy for corn removal surgery based on an individual’s specific case and medical history.
In some cases, hammertoe correction is instead recommended. This may be the cause if you have multiple corns on one toe or if you have long/ bent toes. Hammertoe correction will significantly reduce the risk of the corn recurring in these cases.
What are the Benefits of Corn Removal Surgery?
The benefits of corn removal surgery may include:
- Relief from pain and discomfort caused by corns, allowing for improved mobility and quality of life.
- Removal of the thickened skin and underlying corn, addressing the root cause of the problem and preventing further recurrence.
- Correction of any structural abnormalities of the foot that may be contributing to the formation of corns.
- Prevention of complications associated with corns, such as infection, ulceration, or nail deformities.
- Restoration of foot health and function, allowing for better foot function and comfort in daily activities.
What is the Recovery Process Like?
The recovery process after corn removal surgery may vary depending on factors such as the surgical technique used, the size and location of the corns, and the individual’s healing capacity. In general, the recovery process may involve:
- Following proper wound care instructions provided by the healthcare provider, such as keeping the surgical site clean and dry, and applying prescribed medications or dressings.
- You can carefully mobilise straight away but it is recommended that you try and rest as much as possible for the first 48 hours. You should avoid high impact activities for two-three weeks.
- Avoiding weight-bearing or excessive pressure on the surgical site for a certain period of time, as advised by the healthcare provider, to allow for proper healing.
- Using protective footwear or orthotics as recommended to protect the surgical site and prevent recurrence of corns.
- Following any dietary or activity restrictions given by the healthcare provider to support the healing process.
- Attending follow-up appointments for post-operative evaluation and monitoring to ensure proper healing and address any concerns or complications that may arise.
FAQs
Why Choose Our Clinic for Corn Removal Surgery in the UK?
Our surgeon, Mr Kaser Nazir, has a vast expertise in corn and bursa excision, providing aesthetically pleasing results and as well as reducing pain from footwear rubbing.
The London Foot and Ankle Surgery offers clear pricing for self-funding patients, for patients with insurance we will provide details on how you can authorise.
What is the Corn Removal Surgery Cost?
The cost of corn removal surgery carried out by our surgeon, Mr Kaser Nazir, at 17 Harley Street ranges between £800 – £2400 depending on how many lesions you have on each foot, as well as if you have a corn or a bursa.
Email our team at admin@londonfootandanklesurgery.co.uk today with a picture of your corns and we can provide you with a quote prior to your consultation.
Tendon Transfer
Tendon Transfer can be carried out for both flat foot, high arched foot, unstable ankles and drop foot.
As part of a flat foot corrective procedure, the damaged posterior tibial tendon, which attaches the muscle in the inner calf muscle to the bone on the inner side of your foot, is replaced by a transfer of the flexor digitorum longus tendon, which is found on the inner side of your leg.
For dropped foot and high arched feet with unstable ankles, a range of tendon transfers are performed dependent on case by case.
As part of the flat foot correction when the tibialis posterior tendon fails, an incision is made from the inner ankle so both tendons are exposed. The damaged section of the posterior tibial tendon is removed and replaced with a section of the flexor digitorum longus tendon, this is then sutured into place. The procedure is often carried out alongside a calcaneal osteotomy, gastrocnemius recession or midfoot fusion.
You will require a cast for the first two weeks and will then start to use an Aircast boot for a further four weeks. At two weeks postoperative you should be able to return to sedentary work. Return to sports typically takes 6 months.
You should rest at home for one-two weeks following the procedure. Light exercise can start from six weeks but high impact should not be carried out until three months following the procedure.
This procedure is sometimes carried out alongside a gastrocnemius recession.
Following the surgery you will be placed in a cast to wear for 4 – 6 weeks, this will be followed by the use of an Aircast boot for a further 2 – 4 weeks.
A return to sports can take up to 6 months.
This procedure may be arranged alongside additional surgeries, such as the tendon transfer, gastrocnemius recession and midfoot fusion.
For dropped foot and high arched feet with unstable ankles, a range of tendon transfers are performed dependent on case by case.
As part of the flat foot correction when the tibialis posterior tendon fails, an incision is made from the inner ankle so both tendons are exposed. The damaged section of the posterior tibial tendon is removed and replaced with a section of the flexor digitorum longus tendon, this is then sutured into place. The procedure is often carried out alongside a calcaneal osteotomy, gastrocnemius recession or midfoot fusion.
You will require a cast for the first two weeks and will then start to use an Aircast boot for a further four weeks. At two weeks postoperative you should be able to return to sedentary work. Return to sports typically takes 6 months.
You should rest at home for two-four weeks following surgery. Initially you will require a splint for the first two weeks, this will be followed by four weeks in a cast and then the use of an Aircast boot for a further four weeks.
This procedure may be carried out alongside additional surgery, such as the gastrocnemius recession, tendon transfer or calcaneal osteotomy.
Frequently Asked Questions
What is flatfoot?
In simple terms, a flatfoot deformity is a structural collapse of the arch of the foot. From a multiplanar aspect you will see the arch collapse as well as the heel sitting in an outward position known as valgus and the front of the foot will be visible in a more abducted position as in facing towards your outer leg when you look from a person standing behind the individual. It is important to note that not all flatfoot problems are pathological and different population groups present with different arch heights.
What are the causes of flat feet?
Genetics play a big part in developing or acquiring a flatfoot. Having a low arch alone with no pain or functional disability is not of any concern. However, broadly classifying flat feet there are two main subtypes.
- Congenital flatfoot. This typically is a congenital problem where the most common cause is known as a tarsal coalition. Essentially the hindfoot joints do not separate and are fused resulting in increased stiffness of your foot in a flatfoot position throughout your teenage years and adult life. Typically, symptoms develop between the age of 9 and 15 and can progress from there.
- The second subgroup is acquired flatfoot deformity, and this can be either due to trauma or failure of the tendon and ligamentous structures through injury or disease which results in an acquired flatfoot. The initial presentation is a flexible deformity which becomes rigid over time due to arthritic changes. Some patients have an element of benign joint hypermobility in which case their ligaments are too lax and they develop flat feet which causes generalised musculoskeletal complaints of the lower limb.
What is flatfoot reconstruction?
Essentially it means that the flatfoot deformity is corrected. This can be done in a combination of methods which could involve using extra-articular implants to stabilise the feet, cutting and resetting the heel bone to realign the hindfoot, fusing the midfoot joints to reduce the collapse of the arch, tendon transfer to improve the strength of the arch and function of the foot.
What is minimally invasive flatfoot surgery?
Minimally invasive flatfoot surgery would involve using specialised instruments to cut and reset the hindfoot joints, in particular the calcaneus heel bone to centralise and then use screws through small incisions to allow the repositioning of the heel bone. However, it could also involve a procedure called an arthroereisis procedure and a typical implant used is an HyProCure implant which corrects flexible flat feet through keyhole or minimally invasive surgical intervention.
Can flat feet be corrected with surgery?
Yes. Flat feet can be corrected if they are pathological and cause pain and appear to be progressive in their nature with surgical intervention.
When is flatfoot surgery necessary?
Flatfoot surgery is necessary where there is disease or pathology related to tendons or ligaments that has caused an acquired flatfoot deformity. It is also essential where function is compromised and conservative treatments have failed. It is also essential when there is pain and functional disability.
How long does reconstructive foot surgery take?
The time ranges depending on the surgical intervention required. For example, the HyProCure procedure may only take 10 to 15 minutes whereas a full reconstruction and tendon transfers could take anything from two to two and a half hours.
How quickly can I return to activities after flatfoot construction surgery?
The return to activity would very much depend on the type of surgery. Minimally invasive surgery may require a period of immobilisation for a couple of weeks and then careful mobilisation but full return to activity may still be many months. Significant reconstructive surgery could involve 6 to 12 months before one is returning back to sports or any aggressive activity.
How much does flatfoot reconstructive surgery cost in the UK?
The cost varies again depending on the procedure. It could range from £5,000 to £10,000 depending on the type of operation.
What kind of support do you need for flat feet?
The appropriate shoes which are a rigid trainer with good arch support is essential. One could also wear orthotics or specialised insoles or devices to support their arch during the gait. A range of exercises can also be used to improve strength of the foot.
What exercises are good for flat feet?
The simple exercises that can help include single heel raise exercises to stand and try to elevate your heel and place your weight on the forefoot and to repeat this. Trying to pick a towel up with your toes from the floor or a piece of paper to strengthen your arch. Stretching the calf muscles can also help.
Can you walk after flatfoot surgery?
After a period of rehabilitation one should be able to return back to walking and exercise. This is very much dependent on individual cases in terms of exercise return.
Hallux Rigidus Surgery
The goal of Hallux Rigidus surgery is to alleviate symptoms and improve function at the joint. It is typically recommended as a last resort, should non-surgical measures fail to resolve the complaint.
Types of Hallux Rigidus Surgery
The cheilectomy procedure is carried out to remove excess bone at the big toe, which is caused by osteoarthritis.
During the surgery excess bone and debris will be removed, this will help free up movement in the joint and reduce pain and stiffness.
Initially an incision will be made over the joint of the second toe. The excess bone and fragments are then removed. Range of motion of the toe is checked intraoperatively to ensure sufficient movement.
For non manual work you will require 1 – 2 weeks off from work where you should rest at home, if instead you have an active job then 5 weeks is suggested. At 6 weeks following the surgery, your foot should feel more normal and swelling would have mostly subsided. It is typically suggested that you avoid sports / high impact activities for 3 months.
Surgery to the big toe with the use of an implant may be recommended as a surgical option for arthritis to help reduce pain in the joint.
The implant preserves movement in the toe following surgery.
An incision is typically made at the top or side of your toe. Excess bone growth and fragments will be removed. The bone cut and a silastic implant is used to replace the joint. The implant allows for greater flexibility in the joint.
Typically you will require 2 weeks rest from non manual work, manual work would instead require six weeks. At eight weeks the foot will start to feel more normal and swelling would have mostly subsided. You should wait until three months before undertaking high impact activities.
Fusion of the joint in the big toe can be carried out for severe and painful hallux rigidus (arthritis of the big toe).
An incision is typically made at the top or side of the toe. Excess bone growth and fragments (osteophytes) will be removed. The bone is cut and then fused together with a fixation, such as specially designed screws and plate. This surgery can stop pain when walking and jogging. Following surgery the big toe will not be able to bend
You will require approximately six weeks off for non manual work and eight weeks for manual work. For the first six-eight weeks you will have a plaster cast, followed by the use of an air cast boot for mobilisation. At eight weeks postoperative you the foot should feel more normal and swelling will subside. You should wait until three months postoperative before carrying out sports/ high impact activities.
Should I Have Hallux Rigidus Surgery?
Your specialist will recommend surgery when required and provide detailed information so that you can make a decision on how to proceed.
How Long Does Hallux Rigidus Surgery Last?
Hallux Rigidus surgery usually takes approximately 30 minutes. Though your surgeon will provide a more specific expectation dependent on your case and what operation will be required.
How Long Does It Take To Recover From Hallux Rigidus Surgery?
The majority of healing following surgery happens in the first 12 weeks. Although it does take longer for the swelling to subside and totally return to normal in appearance.
Can You Walk After Big Toe Fusion?
Immediately following the surgery you will have to restrict movement to allow the area to heal. Although you can move a little more after the first 3-4 days with aides. It takes approximately two weeks for you get around without crutches.
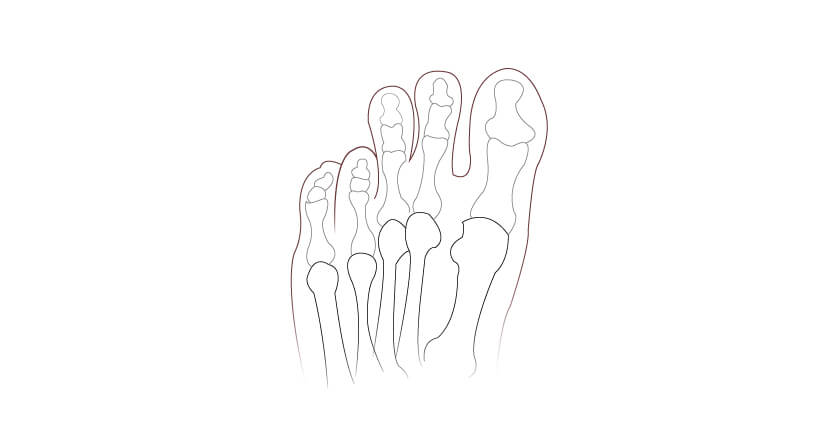
What are Hammer Toes and why do they develop?
A toe is described as ‘Hammered’ when it becomes permanently bent at the first joint. This is due to a muscle imbalance; the toe is normally straight due to the equal forces of the surrounding muscles and tendons, but when the muscles become weak the tendons can pull the toe out of shape.
What does a Hammer Toe look like?
A Hammer Toe is quite distinctive when compared to a toe with natural alignment. Though they can be more or less severely bent:

Treatment for Hammer Toe
Hammer Toes can cause a range of problems, including problems fitting into footwear and corns / callus that result from rubbing against footwear, which can cause painful symptoms. The pain and footwear issues can often be treated without surgery , though surgery can be used to correct the underlying issue.
Day case minimally invasive keyhole Bunion surgery allows immediate weight-bearing with very little postop of pain and quicker recovery than traditional Bunion surgeries. Mr. Kaser Nazir has an international expertise in keyhole Bunion surgery and is one of very few surgeons in the United Kingdom with significant expertise in this operation.
Bunions can cause the whole foot to deform with dislocated toes and painful deformities! Day case operation performed by Kaser Nazir for this patient who travelled from Mauritius to have the operation under a local anaesthetic block in London. #bunion #halluxvalgus #footsurgeon #bunionkinguk #bunionkingoflondon #bunionsurgeon #bunion surgery
Keyhole bunion surgery by Kaser Nazir performed for a painful deformity that progressed quickly. This is the only permanent fix!! #bunion #halluxvalgus #footsurgeon #bunionkinguk #bunionkingoflondon #bunionsurgeon #bunion surgery #bunionspecialist #footsurgery #designershoes #footclinic #kasernazir #toesurgery #footsurgeon #footclinic #beautifulfeet #keyholebunion #harleystreet #cosmeticfootsurgery #chanelshoes #londonfoot
When is Hammer Toe surgery recommended?
If the Hammer Toe symptoms do not resolve with more conservative measures then your specialist may recommend surgery to permanently resolve the issue.
What are the alternatives to Hammer Toe surgery?
Non-surgical treatment of Hammer Toes typically aims to address the symptoms rather than correct the bent toe. These might include:
- Orthotics
- NSAIDS – to manage painful episodes
- Appropriate Footwear – which does not put undue pressure on the toe joints and has sufficient room in the toe box
- Splints or cushioning
Can you straighten Hammer Toes without surgery?
It is possible to reverse the progression of Hammer Toes with conservative measures, such as splints, cushioning and exercises. However, if the toe becomes rigid or fixed in the hammered position, surgery is used to correct the alignment.
Types of Toe Surgery
An incision is made over the top of your toe. A small piece of bone will be removed and then sutured at the joint capsule between the bone ends.
You should rest at home for two weeks following the procedure. You can return to work after two weeks postoperative. At six weeks postoperative you can continue with high impact activities, such as the gym or running.
You should rest at home for two weeks following the procedure. You can return to work after two weeks postoperative. At six weeks postoperative you can continue with high impact activities, such as the gym or running.
An arthrodesis procedure is where the affected joint of the toe is removed and then the bones fused together into a corrected position. This fused joint will no longer move.
An incision is made over the top of your toe. The affected joint is removed and then fused with the use of K-wires. The wires will protrude out the tip of your toe until they are removed at 4-6 weeks post operatively. We also use newer implants that allow an early return to shoes and do not require wires sticking out of the end of the toes in most cases.
You should rest at home for the first three – four weeks following your procedure. You can return to work between three – four weeks postoperatively but need to use a postoperative shoe until the K-wires are removed. At five-six weeks the K-wires will be removed and you will be able to start wearing trainers. At six weeks following your procedure you can return to high impact activities, such as the gym and running.
The main benefit of carrying out toe correction fusion (Arthrodesis) with the use of a Nextradesis or Smart toe implant is the initial recovery. Typically when wires are used you will need to rest at home for a minimum of 4 weeks, with the use of implants you can instead return to work and closed shoes at two weeks following your procedure.
An incision will be made at the top of the toe. The damaged joint is removed and the implant is inserted in its place.
Following the procedure you should rest at home for two weeks. You can then return to work at two weeks postoperative. At six weeks postoperative you can return to high impact activities, such as the gym or running.
The Average cost of Hammer Toe surgery in the UK
We offer a simple fee generator to help illustrate the costs of Hammertoe correction. Please click the below button to launch the quote generator.
The price for Toe Surgery can vary, depending on a number of factors, including:
- The number of toes that need correcting
- Whether the procedure is for both feet or just one foot
- Whether toe implants are used
- If you are self funding or using private insurance; insurance providers often set the fees.
Our team will be able to provide a detailed breakdown of fees following your assessment.
Our Hammer Toe procedures are carried out at The Weymouth Street Hospital who have partnered with Chrysallis Finance to offer monthly payment plans for surgery.
Following your consultation we will provide a full breakdown of your procedure fees so you can arrange your preferred finance option.
Preparing for Hammer Toe surgery
Your foot specialist will advise on a specific toe procedure for your case. You will receive detailed information on the operation prior to the surgery.
There are several things to prepare beforehand. Some important considerations are:
- Let your family and friends know what is happening. This way you will benefit from support such as, checking in on you, helping perform certain tasks that might be hard and keeping you engaged and entertained.
- Prepare your house so that things you will need often are close at hand. This will reduce any need to move frequently. It is often a sensible decision to move your bed to the ground floor.
- Stock up on supplies, such as food and other necessities. This will decrease how often you will need to leave the house.
Hammer Toe surgery before and after
Follow the below link to our gallery to see images of Before and After Hammer Toe Surgery.
Frequently Asked Questions
What to expect after Hammer Toe surgery
You will normally return home on the same day, following the procedure. You will be given instructions on looking after the surgery site and what to expect while recovering. You will be reviewed at important points in time in the subsequent weeks to make sure everything is as expected.
Hammer Toe surgery recovery tips
One of the most important tips for a fast and problem-free recovery is to follow the PRIE regime:
- Protect – you will be advised on how to protect the area while recovering from surgery
- Rest – you will require considerable rest following surgery to allow the area to heal. There will be a very gradual return to activity
- Ice – Icing the area can help with pain and swelling
- Elevate – this will also help with swelling and pain and promote recovery
Recovery time after Hammer Toe surgery
A good rule of thumb is that you will return to normal activity over a period of approximately 8 weeks, though it may take longer for the swelling to fully subside. Your surgeon will provide more detailed information on what to expect from you recovery.
What causes a hammertoe deformity?
Hammertoe deformities can occur when the body tissues that hold a toe in place become unbalanced. The type of shoes you wear, injury, predisposition and certain diseases can contribute or cause hammertoes.
What’s the difference between claw toes and hammertoes?
Both the hammer and claw toes can cause pain and irritation. Claw toes are more likely to affect several toes and all of the joints of the toes are affected causing the toe to contract like a claw. A podiatrist can help you diagnose the precise deformity that you are experiencing.
What’s the difference between mallet toes and hammertoes?
Mallet toes and Hammertoes can often cause similar symptoms, including irritation, discomfort and pain. But they are distinct deformities, a hammertoe affects the middle toe joint whereas a mallet toe affects the upper toe joint nearest to the toenail
How long does it take to recover from hammertoe surgery?
A typical recovery following hammertoe surgery will take place over approximately 8 weeks, with noticeable improvement and return to activity during that time. Initial healing of skin and soft tissue is during the first 10-14 days.
Can you walk after hammertoe surgery?
You can partially mobilize using a postoperative shoe and possibly need crutches but it is important for your recovery to get plenty of rest and keep your foot elevated.
Can you straighten a hammertoe without surgery?
The short answer is unfortunately No. It is possible to slow the progression of the deformity and alleviate symptoms with conservative measures, but surgery is the only way to return the toe to its natural alignment.
Is hammer toe surgery painful?
Hammertoe surgery is carried out under anesthetic, and depending on your particular case this might be local or general anesthetic or sedation. You would not feel pain during the surgery and pain relief can be used during the recovery period.
Do hammer toes get worse with age?
It is certainly possible for a Hammertoe to get worse over time, particularly if you suffer some kind of trauma or wear shoes that aggravate the condition.
How do you treat a mild hammer toe?
There are several treatments available to you, and if the hammer toe is mild it is unlikely that surgery would be recommended. Conservative treatments might include padding, avoiding the use of high heels, pain-relief or steroid injections, among others.
Can you reverse the hammer toe?
Surgery can return a hammered toe to it’s naturally alignment.
How much does hammer toe surgery cost in the UK?
Pricing for Hammertoe surgery will vary depending on factors such as the type of surgery, where it is carried out and how many toes are affected. There is a quote builder available on this page for more detailed information on pricing.
If you have a persistent, infected or recurrent ingrown toenail, or a fungal nail, then your specialist may suggest having the nail partially or fully removed. The procedure can also be carried out with the use of a chemical called phenol, this is applied to the nail bed to stop the nail from growing back, this is typically applied when you have a recurrent issue.
This procedure is usually carried out as a minor outpatient procedure under local anaesthesia, you can leave directly following rather than being admitted into a hospital.
Your foot specialist will start by cleaning the toe and injecting local anaesthesia to either side of the base of the toe. Once numb, the section of the nail or whole nail will be cut down to the base of the nail. The nail will be removed and hypergranulation tissue (scab under the nail) will be removed.
It’s suggested that you take a cab home and rest for the remainder of the day, you can return to non manual work the following day. For the first 3 weeks you will need to re-dress and salt water bathe the toe daily. At two weeks postoperative you can continue with high impact activities.
For self-funding patients, we offer a package fee of £747 with our podiatrist Mr Steven Thomas for a consultation, partial/ full nail removal of one nail under local anaesthesia and postoperative reviews. The fee is £200 for each additional nail removed.
Book online today for an initial consultation and ingrown toenail procedure with Mr Steven Thomas
If you have had a recurrent ingrown toenail, which has previously been partially or fully moved, then your specialist may advise on excision of the nail bed. This will remove the root that contains the cells where the nail grows, this will stop the nail from growing back.
The procedure may be carried out under local anaesthesia or sedation, you will typically be admitted into hospital for half a day. Your surgeon will excise the corner of the base of the nail and remove the root, alongside the affected section of the nail that is causing you pain. This is then closed with stitches.
Following the procedure you should rest at home for 3 – 5 days. You should avoid high impact activities for the first 3 – 4 weeks.
Ingrown toenails can also be caused by a subungual exostosis, this is where a small bone spur on top of the bone underneath your nail. This can cause the nail to lift and push into the sides of the toes. Prior to surgery X-rays are carried out to confirm the presence of the bone spur.
The procedure can be carried out under local anaesthesia or sedation as a day case, you will typically be admitted into hospital for half a day.
Your surgeon will start by making an incision at the top or the end of the toe. The nail may need to be partially or fully removed so that they can access the bone spur, the bone spur is removed by specialised instruments and the wound is then stitched.
You should rest at home for five days following the procedure. Stitches are removed 10-14 days following the surgery. The wound should be soaked in salt water and re-dressed daily until the wound has healed. You will need to avoid high impact activities for three-four weeks.
Booking Your Appointment
For the partial or full nail removal, we can carry out the consultation and treatment on the same day under local anaesthesia with Mr Steven Thomas.
Book online today for an initial consultation and ingrown toenail procedure with Mr Steven Thomas
Mr Steven Thomas is covered by most major insurance companies, excluding AXA PPP and Bupa.
If you are using Bupa or AXA PPP please instead select Mr Kaser Nazir as your specialist, who is covered by all major insurance companies.
For recurring nail issues we would recommend scheduling with Mr Kaser Nazir, who can assess whether excision of the nail bed or the exostectomy procedure would instead be recommended.
Minimally invasive Procedure to Remove Bony Arthritis from Big Toe Joint.
Minimally invasive Cheilectomy
A minimally invasive cheilectomy procedure is used to remove arthritic bony prominence on the top of the big toe joint mostly that develops from osteoarthritis of the big toe joint.
Why is Cheilectomy Done
The cheilectomy procedure generally is used to be done using as an incision of approximately 4 to 6 cm on the top of the big toe joint. The body produces extra bone and bone spurs on top of the big toe joint which causes pain due to impingement and footwear irritation. This is usually a sign of osteoarthritis of the big toe joint.
The big toe joint requires reasonable and pain-free movement to aid good foot function and appropriate propulsion during walking. The minimally invasive Cheilectomy procedures achieves this.
What are the different types of cheilectomy surgery?
Cheilectomy surgery is used to treat early or moderate osteoarthritis of the big toe joint known as hallux rigidus. There are X-ray findings of loss of joint space and cartilage thinning that causes extra bone formation around the joint.
Open cheilectomy
Surgery would involve opening the joint and the capsule using an incision which causes scarring.
Minimally invasive cheilectomy
Surgery only require a small 4 mm incision on the top of the joint through which the whole surgical procedure is performed and hence reduces the risk of scar tissue and a quicker recovery. There is less soft tissue damage and hence less risk of scarring, swelling and post operative pain.
Benefits of minimally invasive cheilectomy?
Minimally invasive cheilectomy allows quicker recovery with only three days of rest. The patients can then wear trainers and start to mobilise as the wound is very small and heals over 7 to 10 days. There is much less swelling and allows early range of motion exercises to maintain and achieve greater range of motion in the joint.
Potential risks and complications
All surgeries carry risks and complications and the main risk with cheilectomy procedure is local nerve irritation which is usually transient. It may well be that the arthritis in the joint progresses over time and it requires joint implant or fusion surgery of the big toe joint in 30% of cases.
Other general risks of any surgery include but are not limited to infection, clots, delayed healing, scar irritation, joint stiffness, continued pain, nerve injury, complex regional pain syndrome. These risks are very small and often mitigated with the expertise to surgeon.
Week-on-week recovery after minimally invasive cheilectomy.
Postoperatively, you would expect that to rest for the three to five days with high elevation of the foot. You can walk no more than 10 minutes an hour. After three to five days the main dressing is removed and the waterproof plaster is maintained. You transition into a trainer and start to walk. You may use a trauma shoe for the first three to five days and week two you can start to push further and start to do some gentle exercises. Running would not possible for four to six weeks usually after minimally invasive cheilectomy. Swelling will typically subside over 8 to 10 weeks where a final result can be determined.
The cost of minimally invasive cheilectomy surgery
Minimally invasive surgery can be performed under local anaesthetic or sedation. The costs vary on the type of anaesthesia. Typically, minimally invasive cheilectomy surgery ranges in the price of £4000- £5000.
Is minimally invasive cheilectomy painful postoperatively?
The pain after minimally invasive surgery is very little. You may need to take painkillers for two to four days postoperatively to manage swelling. However, compare to open surgery your experience will be minimal pain.
What is the difference between cheilectomy and bunion surgery?
Cheilectomy surgery is performed for osteoarthritis whereas the bunion surgery involves cutting and resetting the bone with screw fixation within a healthy joint. During cheilectomy procedure an unhealthy joint is treated whereas with bunion surgery typically there is very little or no osteoarthritis. Also the bump treated with cheilectomy procedure is usually on top of the foot whereas the bunion deformities are mostly on the side of the foot.
How will you diagnosis the hallux rigidus and decide whether minimally invasive cheilectomy procedure is suitable?
Plain X-rays and clinical examination can determine whether there is some healthy cartilage that is still present within the joint. In such cases, a cheilectomy procedure can be very successful as the most of the cartilage remains to be healthy. Should this can also determined with the help of X-rays and should the arthritis be quite progressive in that you have very little or no cartilage then a fusion or joint implants are more appropriate choice of procedure.
How soon can I walk after minimally invasive cheilectomy?
You can walk straightaway for 10 to 15 minutes an hour after the procedure. However, for the first three to five days you should limit this ideally to no more than 15 minutes an hour.
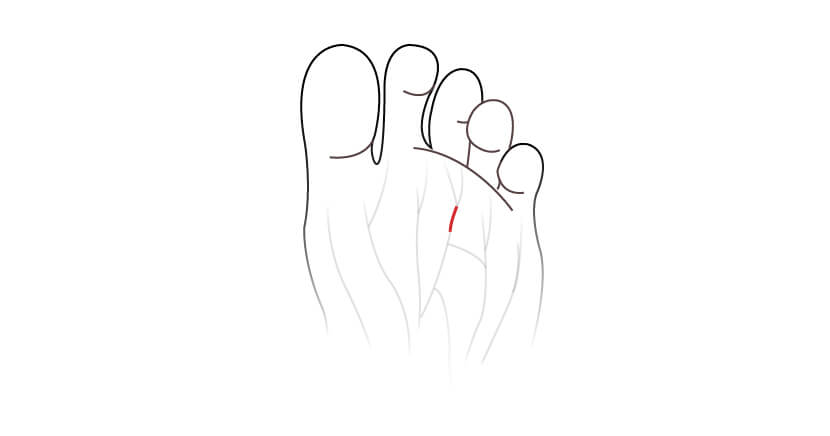
Interdigital Neuroma Surgery
Excision of a neuroma is where part of the damaged nerve that is causing pain and irritation is removed. The procedure may be carried out under local anaesthesia, sedation or general anaesthesia as a day case; you will only need to be admitted into hospital for half a day.
Your surgeon will make a small incision over the top of the foot above the neuroma. Nerves on either side of the neuroma are carefully cut and the neuroma is removed.
What are the alternatives to surgery?
Surgery for Morton’s Neuroma is often a last resort treatment and will be attempted if more conservative measures have failed to resolve the issue.
See non-surgical treatments for Morton’s Neuroma
Morton’s Neuroma Surgery Recovery
Following the procedure you should rest at home for two weeks. For non manual work you can then return work at two weeks postoperative. At six weeks following the procedure you can return to high impact activities.
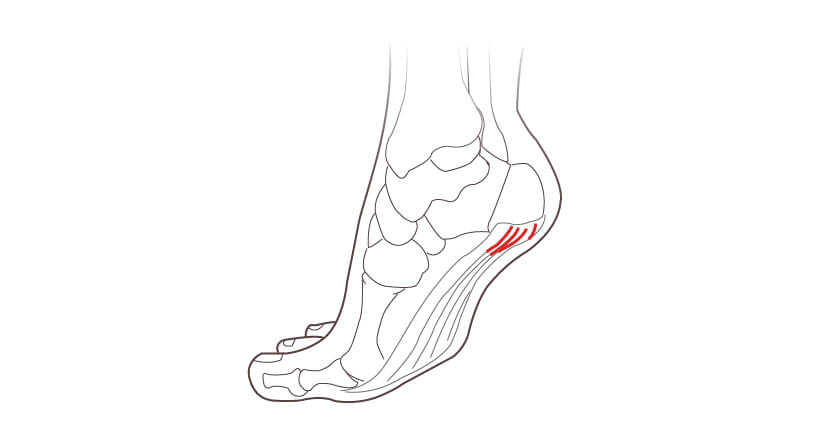
Plantar Fascia Release
Plantar fascia release is carried out to reduce tension and chronic inflammation to the tendon.
A small incision is made on the inside of the heel. The plantar fascia is then detached from the heel, alternatively small incisions may be made on either side to release tension. Damaged tissue may be removed if your foot surgeon finds some present, alternatively the bone may be smoothed, which allows the plantar fascia to heal under less tension.
You should rest at home for the first two-four weeks following the procedure. Between two-four weeks you can return to work. You should avoid high impact activities until three months postoperative.
Plantar Plate Repair
Plantar plate repair may be suggested following an injury to the plantar plates, which are thick ligaments that are located beneath the balls of your feet. This can result in pain and hammertoes, most commonly to the second toe. The procedure involves shortening an elongated ligament or repairing a tear.
Your surgeon will make an incision over the affected toe. The toe is flexed to allow access to the plantar plate, which is then detached. Holes are created in the proximal phalanx and sutured into the realigned position.
Over the first two weeks you should rest at home. At two weeks postoperative you can return to work. At three months postoperative you can return to high impact activities, such as the gym or running.
If surgery is advised to lengthen your metatarsal (and realign toe position), your specialist will initially carry out an X-ray to assess which surgery is most appropriate for you.
This is a relatively common operation where extra length is achieved by inserting additional bone. This process of inserting additional bone is also known as a bone graft. The new bone need only be small, typically up to 1.5cm, the bone can be taken from another part of the body, such as the heel bone.
Once the bone is inserted, the area is stabilised with a bone plate and screws that remain in the foot indefinitely. There is a limit to the additional length that can be achieved with this procedure. As a result this surgery is generally recommended when less than 1.5cm lengthening is required and only for one toe.
You will need to take the first 4 – 6 weeks off from work following surgery. You may require a cast for the first 4 – 6 weeks, following this you may be transferred into an aircast boot for a further 2 – 4 weeks. Full bone healing takes up to three months. Swelling subsides over 6 – 12 months for the final result to be appreciated.
This procedure allows for a greater increase in bone length. The operation involves a precise cut to the bone that does not impede the blood supply followed by attachment of an external fixator device that will stretch the short bone over time. The external device allows you to slowly increase the bone length a little each day, after which the device is removed.
The bone will gradually increase 1mm per day until the desired length is achieved. Once the bone has healed the fixation will be removed between 1 – 2 months postoperatively. Full bone healing takes up to 3 months. You will be in a specialised cast or boot for a period of up to 3 months. Larger deformities in bone length can be corrected using this technique.
Frequently Asked Questions
What is brachymetatarsia?
Brachymetatarsia is a short metatarsal affecting the feet. Usually it can affect one or more metatarsals. The most common metatarsal appears to be the fourth metatarsal and the patient presents with a short or elevated fourth toe. It appears to affect woman more than man.
What are the causes of brachymetatarsia?
The cause of brachymetatarsia is poorly understood. We do know that what tends to happen is that the metatarsal growth becomes stunted and there are theories around this possibly being related to injury but it is often also seen in family members and therefore could present a strong genetic link.
Can brachymetatarsia be fixed?
Brachymetatarsia can only be corrected via lengthening procedures of the metatarsal. This usually involves performing surgery using various techniques that are available.
What happens if brachymetatarsia goes untreated?
Patients often complain of the toe impinging against the shoes and causing irritation. I see patients on a regular basis that are embarrassed by the toe and develop psychological withdrawal from exposing their feet in public. You will often hear stories of them going to a beach and tucking their feet under the sand throughout their holiday. Some patients have never worn opened-toe shoes and others have never been comfortable in front of their partners to expose their feet. The impact appears to be wide and varied.
What are the treatment options for brachymetatarsia?
The treatment options have always been either to wear roomy deep shoes if one does not elect to have surgery. In the past all the techniques have involved amputation of the fourth toe or the affected toe which had generally a quick recovery period but in my opinion would lead to disfigurement. Surgical lengthening of the metatarsal is the ideal solution.
In terms of surgery there are two mainstream treatment options. The first one being a single-stage lengthening procedure which involves cutting and lengthening the bone and using a bone graft either from a patient or bone bank or artificial bone to interposition between the graft to maintain the length. Screws and plate specially designed for lengthening are used to stabilise the lengthened bone and the bone graft until healing has been achieved.
The other common technique is external fixator. The fixator is placed on the bone and held with specialist wires. The bone is cut and slowly lengthened over a few weeks. The fixation is then held in place until the bone healing has been achieved on X-rays.
How do you fix brachymetatarsia without surgery?
It is not possible to fix brachymetatarsia or lengthen the bone without surgery.
How long does it take to recover from a toe lengthening (brachymetatarsia) surgery?
The length of recovery typically depends on the type of procedure.
The single stage lengthening procedure would involve you to be in a cast for five to six weeks postoperatively with no weight on the foot until some bony consolidation is seen where the bone graft is placed to lengthen the bone. Following that patients typically will be in a walking boot for another four weeks. At 10 weeks postoperatively they are allowed to return to trainers. However, the swelling will continue to subside typically for up to six months and can even take up to a one year. The toe becomes stiff after the surgery and will require some therapy to try to regain the range of motion.
The external fixation technique requires you to be in a cast for approximately six weeks. The first three weeks are typically where the lengthening is taken place by daily rotation of the dials on the external fixator. The fixator is then held in place for anything up to three to six months depending on bone healing. Most people can have the fixator removed at three months but may well still be partially weightbearing on the foot. Complete healing can take approximately one year.
When can I walk after brachymetatarsia surgery?
Walking after brachymetatarsia surgery in both cases will not be allowed for first six weeks. Following this one can place weight but may still be in a protected boot for a prolonged period.
Is brachymetatarsia a birth defect?
There is still a debate as to whether it is or not. It could be a defect of the growing skeleton or may well be due to genetic predisposition.
What is the cost of brachymetatarsia surgery in the UK?
The London Foot & Ankle Surgery Clinic has arranged package prices for both single stage and external fixator techniques and they typically range from £7,000 to £10,000 per foot. Only one foot can be operated on at a time due to the level of immobilisation required in a cast postoperatively.
Fifth Metatarsal Osteotomy
A fifth metatarsal osteotomy is often used to treat a Tailor’s Bunion (Bunionette).
An incision will be made around the Bunionette, the exact location will depend on the shape of the bony prominence. Via this single incision, excess bone growth (the Bunionette) is removed, which is followed by a shifting of the head of the bone inwards to decrease the width of the foot. A screw is used to keep the newly positioned bones in place while they heal.
Recovery following surgery will take place over 6-8 weeks, with a complete return to strenuous activity, such as sports, at 3 months. You can return to work between 2 – 6 weeks after the operation, depending on how active your job role is. You can typically return to driving at 6 weeks.
Average cost of Tailors Bunionette surgery in the UK
We offer a simple fee generator to help illustrate the cost of Tailors Bunion correction. Please click the below button to launch the quote generator.
The cost of Tailors Bunionette surgery will vary across the UK, depending on a number of factors and the type of procedure that is recommended.
Our team will be able to provide a detailed breakdown of fees following your assessment.
Toe shortening is a surgical procedure that reduces the length of one or more toes. The surgery involves removing the bone or the end joint of the toes to reduce the overall length of the toe and to improve footwear fitting. It is often used for cosmetic purposes also.
Long toes can also result in toe deformities in the long-term such as hammer toe or mallet toe deformities which involve a similar procedure.
What is Toe Shortening?
Toe shortening is a procedure to shorten the overall length of the toe by removing bone or the joint within the toe to correct deformity or for aesthetic reasons.
What is a Long Toe?
A Morton’s toe is often called a long toe where the second toe is longer. This is a genetic foot type. Often you find that some patients have very long toes that are genetic and do not fit regular shoes and cause corns and calluses as well as deformities.
What causes Long Toe and its symptoms
The symptoms are usually caused by poor footwear fitting where the long toe bends in the toes and causes impingement.
What are the common reasons for Toe Shortening
Most patients want toe surgery to fit into appropriate footwear whilst others want more cosmetically staircase structure of toe lengths.
The Average cost of Toe Shortening Surgery in the UK
We offer a simple fee generator to help illustrate the costs of Toe Shortening Surgery. Please click the below button to launch the quote generator.
The price for Toe Surgery can vary, depending on a number of factors, including:
- The number of toes that need correcting
- Whether the procedure is for both feet or just one foot
- Whether toe implants are used
- If you are self funding or using private insurance; insurance providers often set the fees.
Preparing for Toe Shortening.
It is prudent to consider risk versus benefit when considering toe shortening surgery. It takes a long time for total recovery and the swelling typically would subside over three to four months’ period and patients would often be counselled regarding the process. The final results may not be evident for 16 weeks or longer in some cases.
Toe shortening week-on-week recovery
Toe shortening is performed either with special wires that hold the bones together and I remove after five to six weeks or internal screws. The final outcomes are the same and results would not differ between the two techniques but the postoperative recovery is different.
With both procedures you will require two weeks of relative rest with high elevation and no more than 10 minutes an hour of mobilisation. Between weeks two and six if you use wires then you will maintain postoperative shoe as the K-wires protrude out at the end of the toes. However, with screw fixation it may be possible to return to rigid trainers sooner.
With K-wires they are removed at six weeks postoperatively. At that point, you can start to do exercise and increase the activities. With screw fixation you will return to shoes quicker but the exercise will still not be allowed for six weeks whilst the toe bones heal.
The swelling will continue to subside over a 6 to 16-week period. You may not be able to wear all your smart shoes during that period.
Toe Shortening risks and complications
Risks and complications include but not limited to infection, clots, delayed healing, scar irritation, non-union, removal of screw, floating toe, malunion where the toe unites abnormally, complex regional pain syndrome.
Verruca Removal Surgery
If more conservative measures fail to resolve your verrucae, surgical removal may be recommended. There are many ways to achieve this, at our clinic this will typically involve either of the following:
Verruca Excision is a minor surgical procedure used to remove plantar warts.
The procedure involves the use of local anesthetic to numb the area. Following this the verruca is scraped away using a curette. Depending on the size of the verruca a small stitch may be used while the area heals.
A Verruca Excision be carried out in an out-patient setting, meaning you can return home the same day with no overnight stay in hospital.
Recovery can take between 1- 2 weeks, depending on the number and size of the verrucae.
Electrosurgery can be used to treat Verrucae if over-the-counter treatments have failed to resolve the problem. It is a minor surgery that makes use of a machine called a Hyfrecator.
Hyfrecation involves the use of electrical current to burn away the verrucae. This is often used in conjunction with surgical excision; the wart is excised surgically and any remaining wart is then removed with the Hyfrecator.
The area heals quickly over a matter of weeks (usually 2-4 weeks). Sensible shoes and as much rest as possible will help the healing process. You can normally go back to work soon after the procedure. Your specialist will advise you on this.
Schedule a consultation with Mr Steven Thomas for verruca removal, Mr Thomas is covered by most major insurance companies excluding AXA PPP and Bupa.
We have clear pricing for our self-funding patients:
- £750 consultation and excision of one verruca with Mr Steven Thomas
- £250 for each additional verruca
For clusters or larger verruca we have the following pricing:
- £150 consultation with Mr Steven Thomas
- £1250 small cluster or one large verruca excision
- £1700 large cluster or two large verruca excision
If you are covered by AXA PPP or Bupa, arrange a consultation with Mr Kaser Nazir who is covered by all major insurance companies.